David Nelson’s condition started to decline when the pandemic hit.
Nelson, a resident of the memory care unit at Havenwood Senior Living, has lived with Parkinson’s disease and memory loss since early 2015. In March, when Nelson’s wife was no longer allowed to visit, he started to have hallucinations and would become agitated. The nurses at Havenwood suggested moving Nelson to a geriatric psychiatric facility.
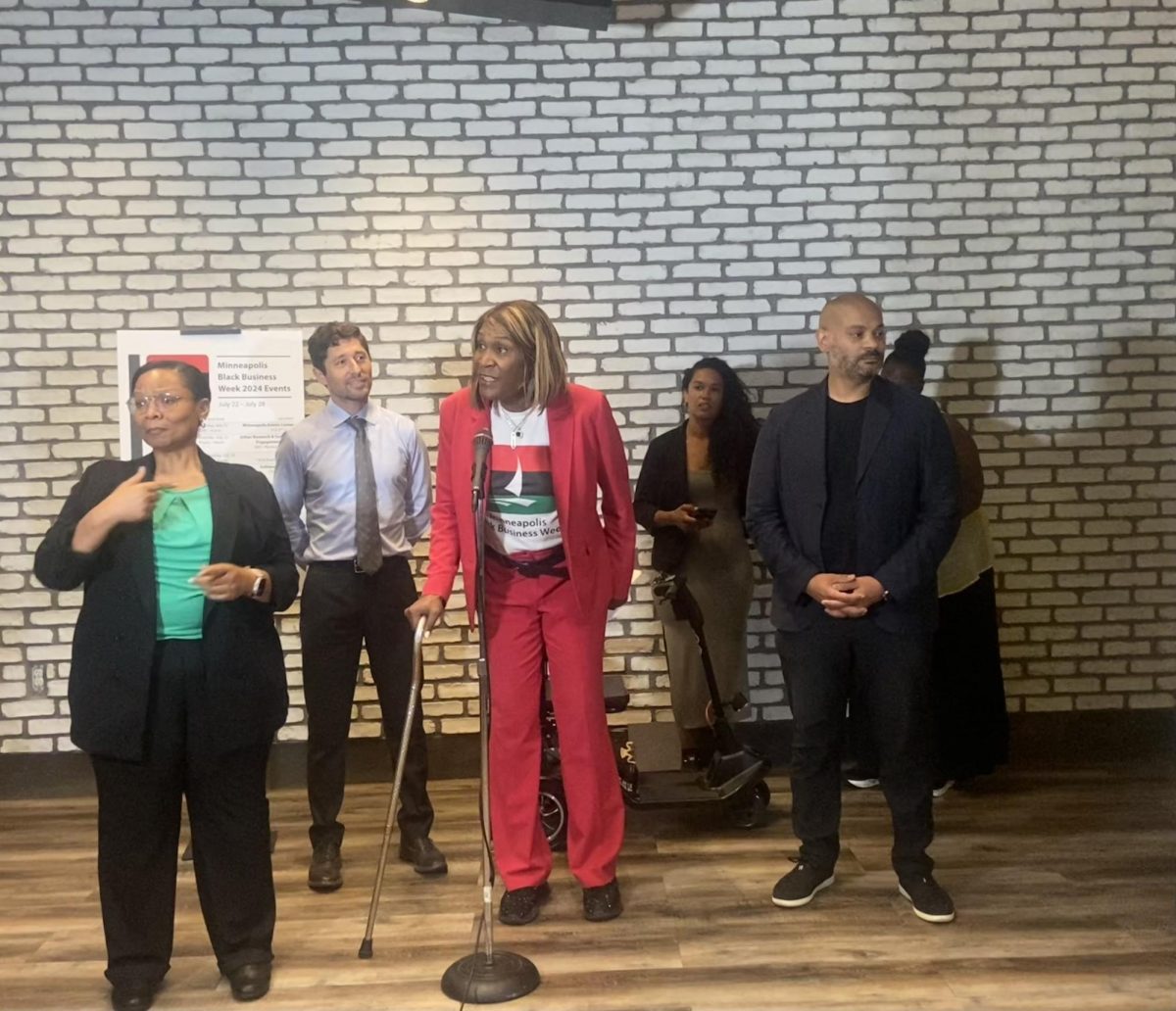
This move could have had negative health impacts on Nelson, said Tracy Keibler, the founding and executive director of START Senior Solutions, an elder education and advocacy organization in Eden Prairie.
“He was so frail. The transport, getting into a new setting, the way they radically work on his medications and things … everyone that I’ve talked to said this would not have been a good outcome,” Keibler said.
As the United States’ population ages, Alzheimer’s disease and related dementias (ADRD) are becoming a growing problem, according to Dr. Sayeh Nikpay, an associate professor in the University of Minnesota’s School of Public Health.
There is no treatment for ADRD, but access to specialty providers like neurologists, geriatricians and psychiatrists can improve the patients’ quality of life and care. However, not everyone has equal access to quality care, according to a recent study by Nikpay and a team of researchers from Vanderbilt University in Tennessee.
When Nelson’s wife, Karen Nelson, called Keibler asking for recommendations for a good geriatric psychiatric facility, Keibler instead recommended a visit to a neurologist.
“He and I had a phone conversation for probably half an hour,” said Karen. “And he said, ‘Let’s just increase a couple of the meds just a tiny bit and see if that helps.’ And I do think that that helped. Just a little increase of his meds helped him.”
In a study published late last month in the Journal of General Internal Medicine, Nikpay and her colleagues used data to analyze access to specialty providers for patients with ADRD.
While other research in this area has used small clinical studies, Nikpay’s research is unique because the team used large data sets to identify disparities in care.
Using medical record claims data from the Southern Community Cohort Study, a study of approximately 85,000 primarily low-income participants living in 12 southeastern states, the researchers identified patients using ADRD care and linked them to specialized providers.
From there, the researchers tested for disparities among patients with ADRD. They tested whether patients with access to more resources, including having a higher socioeconomic status or level of education, had better access to specialized providers, such as geriatricians, neurologists and psychiatrists.
The data found that people with lower socioeconomic statuses and residents living in rural areas had less access to specialized providers.
Jenna Pogorels, senior program manager for the Alzheimer’s Association’s Duluth, Minnesota office, said that the lack of aging specialists in rural communities could be a barrier to care.
“Many [patients] travel many miles and many hours to get to Duluth to find the nearest neurologist or neuropsychologist who might be able to provide a diagnosis more specifically,” Pogorels said. “When you have a lack of population, you have a lack of resources and things popping up, and [the resources] can be spread thin in some of the rural areas.”
While urban areas rely on the medical system or family networks, rural communities rely on everyone — the letter carrier, the local coffee shop owner or the bank teller — to be aware of ADRD and how they can help people.
In general, accessing geriatric care is challenging, said Dr. Joseph Gaugler, a professor in the School of Public Health and the director of the Center for Healthy Aging and Innovation at the University.
“It’s estimated that we have to triple the number of geriatricians who are practicing in 2019 to effectively care for older adults who have Alzheimer’s by 2050,” Gaugler said.
Our current healthcare system is focused on episodic care, or charging and billing for expensive services and procedures, Gaugler said.
“[Optimal geriatric care] is really predicated on time: time, multidisciplinary teams and engagement — not only with older patients but families as well,” Gaugler said. “And, in a largely fee-for-service healthcare system, that kind of care is not rewarded.”
Without regular support from specialty providers, Gaugler said there is an increased risk of adverse health effects. Medication mismanagement and lack of access to psychosocial support for caregivers are two main concerns Gaugler raised.
Patients with ADRD also do poorly when they end up in the emergency room, Nikpay said. Better access to preventative care in the outpatient setting could help mitigate negative outcomes.
“They’re more likely to die, they have worse health outcomes, they’re more likely to get admitted to a nursing home after their stay,” Nikpay said. “Maybe having better management in the outpatient setting, … you might be less likely to end up in the [emergency department].”
Nikpay also said regularly seeing a specialized physician could help patients better identify resources to help prevent cognitive decline.
The next steps in Nikpay’s research include looking deeper into socioeconomic disparities in care and their various health consequences.
She said, “We’re thinking about how we can take these results to the next level and say something about what happens to health data and to what’s driving the disparities.”



















Amy Grahams
Mar 2, 2021 at 4:09 am
As time passed i had other symptoms; hand tremors, restless sleep, muscle weakness, cognitive decline, voice spasm, stiff achy right arm and ankle. At 60 i was diagnose of PARKINSONS DISEASE, i was on Carbidopa and Pramipexole for two years, they helped alot but not for long. As the disease progressed my symptoms worsened, with my neurologist guidance i started on natural alternative PARKINSONS DISEASE treatment from M.H.C. (Mayaka Natural Clinic), the treatment worked very effectively, my severe symptoms simply vanished, i feel better now than I have ever felt and i can feel my strength again. Visit ww w. mayakanaturalclinic. c om. c om. My neurologist was very open when looking at alternative medicines and procedures, this alternative parkinson disease treatment is a breakthrough.