Many restaurants are closed, public gatherings are prohibited and classrooms at the University of Minnesota sit empty, despite it being the middle of the semester. It is not 2020 — it is fall 1918, and the influenza pandemic is in full force.
World War I was mobilizing around the globe as a severe influenza outbreak, which most know as the “Spanish flu,” spread worldwide, infecting millions. The University had become home to a military training camp for more than 3,200 soldiers and delayed classes in the hope that the outbreak would die down. Hospitals were overfilled and supplies scarce.
Although the world looks vastly different in 2020 than it did a century ago, many of the same strategies used today to reduce the spread of COVID-19 were also enforced then.
The University’s Board of Regents in 1918 originally delayed classes until Oct. 2, so the military training camp — the Student Army Training Corps — would have time to acclimate on campus.
But in the wake of influenza spreading to Minneapolis and 1,000 confirmed cases in the city within the first week of the virus’ arrival, the University delayed the first day of classes for those in the SATC to Oct. 9 and until later in the semester for civilian students.
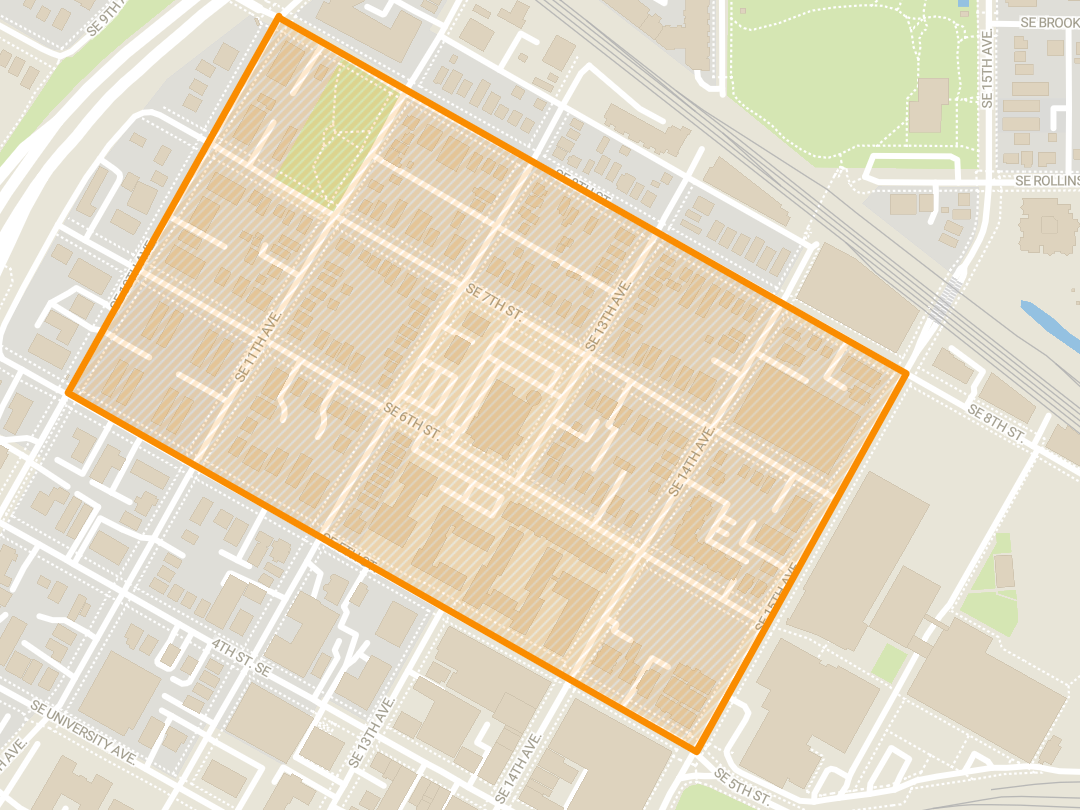
Health organizations serving SATC soldiers-in-training resided in empty fraternity houses on University Avenue. It is thought that these young men brought the flu to Minneapolis from their war travels. In the early days of the influenza outbreak in the city, a majority of the cases reported were soldiers in the SATC and nurses at the University hospital.
The University campus was at the center of the city’s outbreak. In all, 2,000 University students, the majority of whom were soldiers, contracted the disease. Twenty students died.
“In the years to come, when some historian seeks to portray the life and works of the University of Minnesota, he will in all probability set down the year 1918–19 as the most unusual period in all the early history of this institution,” wrote then-University President Marion LeRoy Burton in his annual report. “As a matter of fact, the University as such ceased to function and in its place was established a military camp.”

College life in the middle of a pandemic
Hundreds of new cases and around a dozen deaths were reported each day in Minneapolis by mid-October. Like today, religious buildings, schools, theaters and other public places were closed to slow the spread of influenza.
In a lucky coincidence for the University, 1918 was also the year the University Health Service, now Boynton Health, was created. It saw 100 patients each day and served many students who were isolating themselves in their dorms or barracks.
Like COVID-19, the 1918 influenza virus targeted respiratory function and ultimately led to severe pneumonia in many cases. It easily spread from one person to another and most commonly killed children, those ages 20 to 40 and those over 65.
The influenza’s impact on young adults took many by surprise.
“During the last weeks of September influenza struck Minnesota with an almost explosive violence. I shall never forget the first victim at the University, a handsome, robust, young second lieutenant. In less than a week his body was sent home,” wrote John Sundwall, director of the University Health Service in 1918.
Not only do COVID-19 and the 1918 influenza parallel in their symptoms, but also in their naming.
Many know the 1918 influenza pandemic as the “Spanish flu,” even though the disease did not actually originate in Spain. Earlier this month, President Donald Trump called COVID-19 the “Chinese” virus, although the virus has spread worldwide, and the United States currently has the highest number of cases.
University doctors and nurses were helping with the war effort, so the major source of medical care at the time was student nurses and medical interns. Eligible male students were drafted to aid in the war, so female students took on many responsibilities.
Pearl McIver, a nursing student during the pandemic, worked at the University Hospital’s pediatric unit to care for sick children. She wrote about her first day on the job, documenting the chaos she encountered.
“There were 30 children varying in age from 2 to 10 years,” McIver wrote. “All were desperately sick, many had been picked up by policemen from homes where the parents were found dead or in a dying condition from influenza.”
McIver said on that night, she took off her mask and nursing cap to “look more like a human being” for the children and rocked them to sleep, despite contact being strictly prohibited in the unit.
Widespread sickness, limited information
War is about strategy. No country wanted to give another an advantage during World War I, and many, including the U.S., did not want to publicize the number of influenza cases or deaths for fear that countries would view them as weak, said Jeremy Youde, the University of Minnesota Duluth’s College of Liberal Arts dean and a global health politics and policy researcher.
“Public health can never be entirely separated out from politics and economics and the larger social forces that are going on in the world,” Youde said.
Large gymnasiums and indoor gathering places were converted into makeshift hospitals. There really was no standardized treatment for influenza, just treating the symptoms the patients presented, Youde said.
In addition to the deadly influenza pandemic and World War I, northern Minnesota also experienced a deadly forest fire near Cloquet and Moose Lake that killed about 500 people. This displaced hundreds of Minnesotans and many moved into temporary housing, which turned into a hotbed for spreading influenza, said Curt Brown, author of the novel “Minnesota 1918.”
“If you were lucky enough to survive the fire, you were crammed into evacuee housing, where you became a good candidate to catch the flu because you were so tightly packed together,” Brown said. “And on top of all that, of course, we had World War I dragging to a bloody close in Europe … it really was a trifecta of woe.”
‘Trying to restore a sense of normalcy’
Once the war came to its conclusion in November 1918, the U.S. government and its citizens tried to return to normal. But shortly after World War I ended and some restrictions to prevent the spread of influenza were lifted, another wave hit.
After three deadly waves of influenza, businesses reopened and many people chose to not discuss the horrors they witnessed, Youde said.
Although the 1918 influenza virus was something the world had not seen at the time, numerous pandemics hit the nation prior to World War I, so in a way, the U.S. should have been more prepared, he said.
Some experts argue the same thing today as the number of COVID-19 cases continues to climb.
“In order to stop the spread of a disease, we need to really prioritize communication and trust,” Youde said. “We’ve seen these sorts of inconsistent messages, and it doesn’t seem like everyone is singing from the same hymnal, if you will.”
Today, as many hospitals in the U.S. are dealing with personal protective equipment and hand sanitizer shortages, Brown wonders if America should have seen this pandemic coming.
“I think we were caught flat-footed,” Brown said. “If we had leaned on history a little more, maybe we wouldn’t have been so ill-prepared for this.”