For health providers, keeping track of patients with HIV has
proven troublesome.
A University of Minnesota study — funded by the National
Institutes of Health — looked into the impact state HIV surveillance data could
have on keeping doctors in contact with patients who have stopped seeking care.
The analysis, presented on Nov. 2, found that Hennepin
County Medical Center (HCMC) could reduce searches for HIV patients by about 30
percent if the hospital had access to case data, said Eva Enns, the study’s
lead researcher and assistant professor at the University.
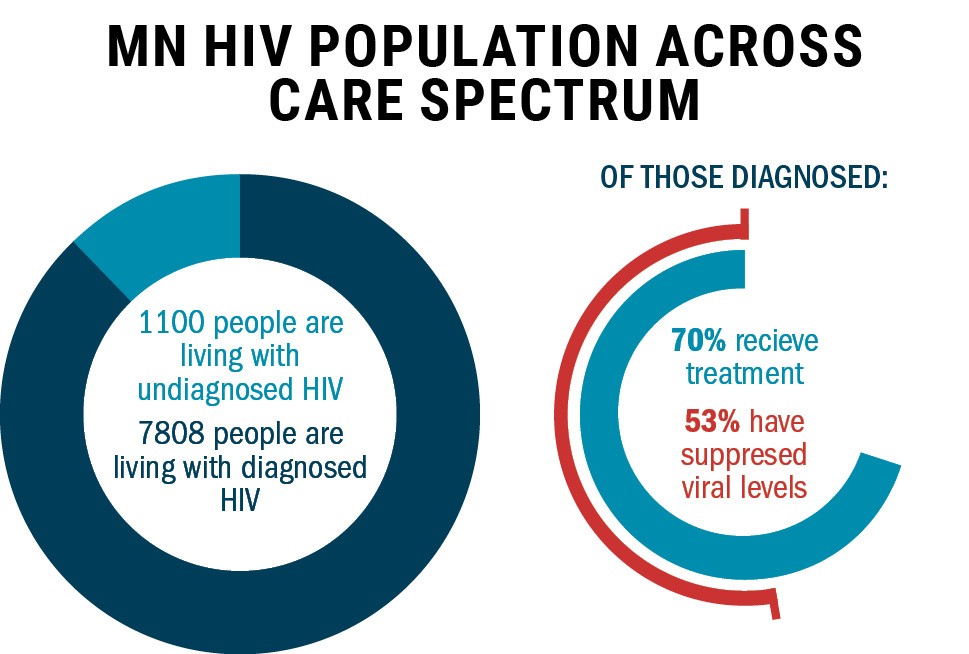
The data, which is collected by the Minnesota Department of
Health (MDH), measures the prevalence of the disease by tracking cases, death
records and provider care data.
Dr. Keith Henry, who works at HCMC, said HIV patients who
don’t follow up on care are a common problem.
He said while providers worry about their patients’ health,
they’re also concerned about the risk of viral transmission.
“For those patients in our clinic who are in care regularly,
87 percent of our entire population in care are suppressed and undetectable,”
Henry said.
Reasons patients stop seeking care might include switching
providers, moving, personal life instability or death, Enns said.
“It may be that they have other priorities in their life
than their HIV care,” she said. “Their HIV typically is going to be
asymptomatic.”
But without easier access to state surveillance data, tracking
patients is difficult for providers, Henry said.
Access to this data would help clinics allocate resources
toward patients who are truly out of care, rather than those who’ve switched
providers or moved away, Henry said.
“It would allow [providers] to have a better sense of their
current caseload,” Enns said. “They would know which patients in fact they are
no longer seeing because they’ve left the state or they’ve died and so on.”
But Allison La Pointe, HIV surveillance coordinator for MDH,
said some of the blame for the lack of data access falls on the providers.
“[Providers] rarely take advantage of calling the health department
to ask about patients,” she said.
MDH, however, wouldn’t disclose the patient’s information to
providers if the individual was receiving care elsewhere, said La Pointe, a
collaborator on the study.
Still, Henry said he’d like to see more collaboration
between MDH and healthcare providers to find and reintegrate these patients
into care.
From there, he said he’d like to see efforts to improve care
to prevent patients from leaving.
Enns said she plans to build upon this research through
examining what factors contribute to a patient’s decision to stop seeking care.
“The next phase of this is to look at barriers to care,” she
said. “So, reasons that people might not engage in care as frequently as …
recommended.”