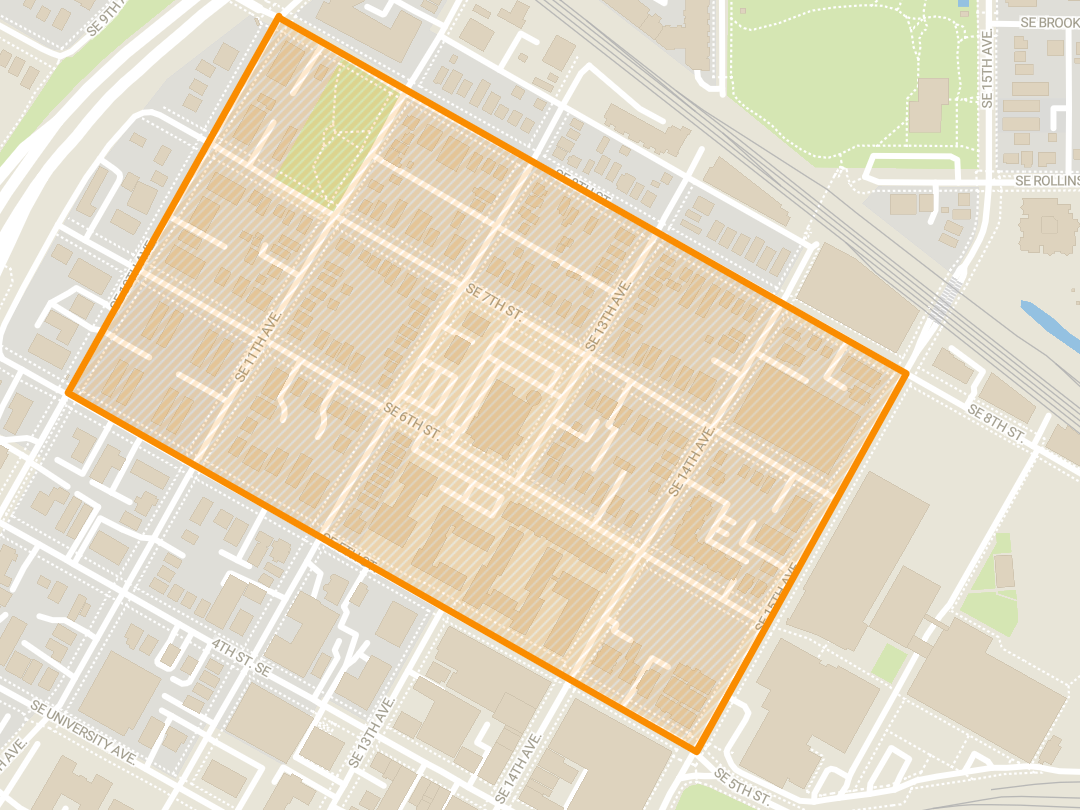
University of Minnesota researchers are trying to create new, less toxic therapies for pediatric leukemia.
Current therapies for leukemia can leave children with short- and long-term side effects. Researchers began this work early last month after they were awarded a $350,000 five-year grant for their study from the National Cancer Institute.
“Our therapies have certainly improved over the last years and decades, but again, we’re not curing all children. Meaning they’re dying from leukemia, and the children we’re curing — they’re living with the long term effects,” said Peter Gordon, a researcher and University assistant professor of pediatrics.
As a pediatric oncologist, a doctor who treats cancer in children, Gordon said he sees both the successes and the shortcomings in current leukemia therapies. The question was whether researchers could improve those therapies.
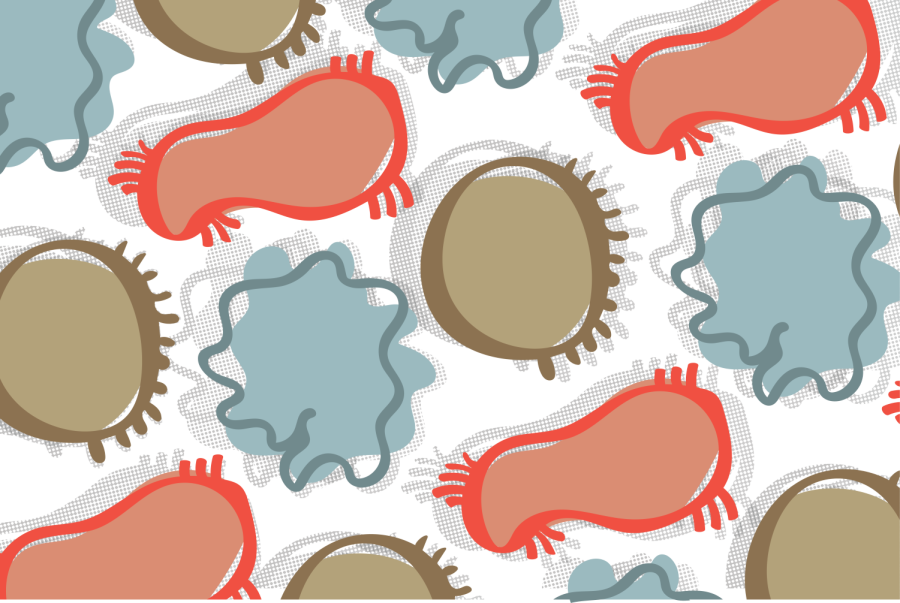
Leukemia is a systemic disease that starts in the bone marrow. It is a cancer of the white blood cells, which normally fight infection, making them grow out of control. The bone marrow produces cancer cells, which allows the cells to infiltrate any tissue in the body, disrupting their function.
“The biggest problem of the current therapies [is] that they are very non-specific and target all rapidly dividing cells,” he said. “There are a lot of cells within our body that grow rapidly. Those can also be targeted by chemotherapy.”
When other cells are targeted, other lifelong issues can arise, such as cardiac, behavioral and metabolic problems.
“It’s not just enough to cure them of their leukemia. I think we need to start to really ask, can we cure them, but do it in such a way that they can go on to live long, healthy lives without these chronic medical problems that we can really directly trace back to the therapy they received,” Gordon said.
Researchers know that the normal interactions between the cancer cells and normal cells in the body protect the cancer. Gordon’s lab is interested in disrupting these interactions between the cancer cells and the body.
“The initial treatments can work but oftentimes only for a time, and then there’s a relapse and the first line of treatment has failed now. In many cases, there’s not a second line of treatment,” said David Odde, a researcher and University professor in the Department of Biomedical Engineering.
Despite 90% of childhood patients achieving control of the disease, relapse after initial treatment is common, said Lee Greenberger, the chief scientific officer for the Leukemia and Lymphoma Society in an email to the Minnesota Daily.
“A second round of therapy with drugs that might not encounter resistance are needed,” he said in the email.
CAR-T immunotherapy is one type of therapy that uses an altered type of T cell to fight cancer. Greenberger said it is important to make better CAR-T therapies that are less toxic and more effective, among other things.
“There’s a great opportunity to connect biophysical modeling approaches and images to understanding the biology … [and] improving the treatment for kids who have relapsed with leukemias, and I’m excited about that,” Odde said.