After years of testing on mice and dogs, a team of University of Minnesota researchers treated their first human patient for glioblastoma, an aggressive brain and spinal cancer, late last month.
There are several existing drug therapy options for cancer, such as Keytruda, Opdivo and Libtayo, that work to strengthen the immune system. However, this new treatment has a make-up and tumor suppression that is new to the medical field, in addition to activating the immune system to fight cancer cells.
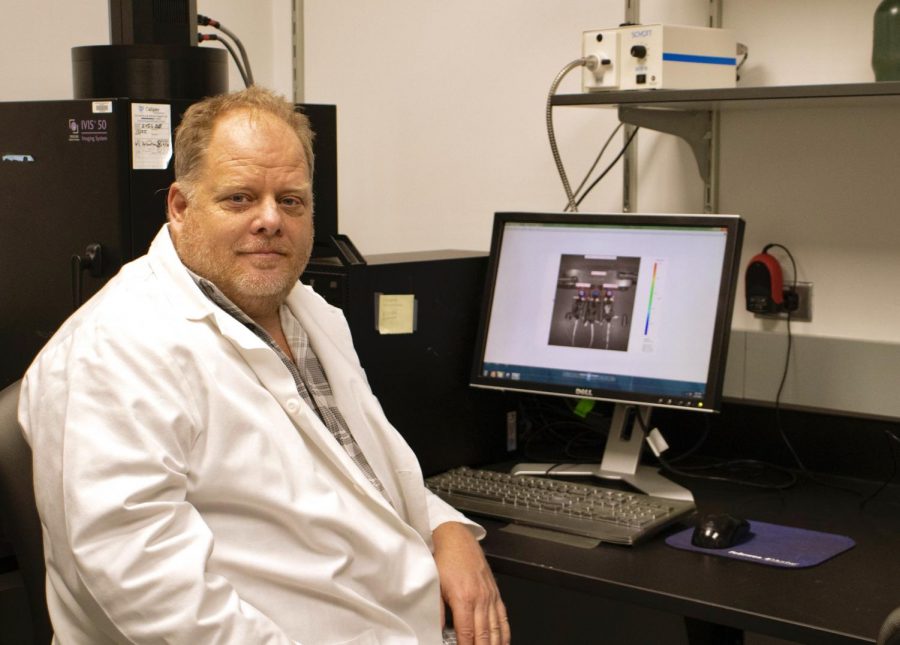
Dr. Michael Olin, an associate professor in the oncology division of pediatrics at the University, has been working on this new treatment since 2012. “This is my baby,” he said.
“It’s very translatable to other diseases, to other cancers and potentially even infectious diseases,” Olin said.
Phase one of the human trial
Phase one of three of the trial will last about two years and treat up to 18 people. Three patients will be treated at a low dose before the trial is able to move onto a higher dose with three new patients. The team is taking a slower approach to testing the treatment due to guidance from the Food and Drug Administration.
“We’ve done other trials with what we call a rapid escalation design but [the FDA] thought that it was inappropriate given how new this drug is and not knowing exactly what the side effects would be,” pediatrics professor Dr. Christopher Moertel said.
Olin and Moertel have both remained at a distance from the trial so as to not to influence its outcome or analysis. Assistant professor in the Department of Neurology Dr. Elizabeth Neil, who started the previous trials in canines, is currently leading the human trial.
If the treatment is proven safe in three adults, the researchers can then expand to a pediatric trial. Despite the versatility of this new treatment, Olin said they chose to focus on brain cancer first because it is the cancer with the highest mortality rate for children.
Currently, the treatment is given in the form of an injection at the base of the neck where the lymph nodes associated with the brain are accessible. The location of the shot is specific to treating brain cancer. The treatment frequency is slowly reduced over time as the body starts to build immunity.
During phase one of the trial, the therapy will only be administered to volunteers who have already been treated for glioblastoma and are now seeing it return. Individuals in that situation are in the greatest need of help, Moertel said.
So far, the team has not seen any side effects from the animal or early human trials, Olin said.
When tested on mice in previous trials, the treatment was successful in fighting breast tumors, brain tumors and melanoma. In dogs, approximately one in five brain tumors were permanently eliminated.
Olin and Moertel started the company OX2 Therapeutics in 2016 to raise money for the trial. External investments allowed them to move forward much more quickly than if they had solely relied on grants and philanthropy to fund their technology, Moertel said.
How it works
In 2018, researchers James P. Allison and Tasuku Honjo were awarded a Nobel Prize in Physiology or Medicine for their research on how cancer uses immune checkpoints to make the immune system less aggressive. Cancer is constantly sending out chemicals to inhibit T-cells, a type of white blood cell essential to the body’s immune system. When immune checkpoints are blocked, T-cells are able to fight cancer cells more effectively.
Building off of Allison and Honjo’s work, Olin discovered a simpler way to downgrade immune checkpoints by using a peptide chain to activate the immune system and control the inhibitors so the cancer cells are unable to fight back. This is a different method than the use of antibodies commonly used in other immune checkpoint treatments.
Olin’s revelation came from a protein shed by cancer cells called CD200. The protein inactivates T-cells and fights against immune system responses. Current cancer treatments are full of this protein, according to the OX2 Therapeutics website.
If the new treatment is shown to be safe by the FDA in phase one of the trial, the researchers will go on to test the treatment’s efficacy. During phase two, the trial can treat a larger number of patients. Moertel estimated about 60 people will be eligible when the time arrives. And finally, in phase three, the treatment will be compared to the most effective existing therapies in the field: radiation and chemotherapy.












James Peters
Jan 27, 2021 at 9:41 pm
A link to the trial (in rGBM) https://clinicaltrials.gov/ct2/show/NCT04642937