A surgeon at the University of Minnesota partnered with graduate students and faculty to develop an affordable, reusable and environmentally sustainable surgical tool for repairing pelvic floor prolapses in low-income countries.
Dr. Rahel Nardos, the director for Global Women’s Health within the Center of Global Health and Social Responsibility, said there was no reusable, affordable and easy-to-use device to treat late-stage pelvic organ prolapse in low- and middle-income countries.
Growing up in Addis Ababa, Ethiopia, Nardos said it was difficult to access good health care. She said she wanted to create a new pelvic floor device to help women in low-income countries receive quality health care.
“I can do a little to contribute within my power,” Nardos said. “We all have the power to do something and challenge the system.”
Nardos, an associate professor in the Division of Female Pelvic Medicine and Reconstructive Care at the University, said pelvic organ prolapse is common among women, especially after childbirth.
12% of women undergo a surgical correction for pelvic floor prolapse, according to a study published by the National Library of Medicine.
Pelvic floor prolapse is the descent and protrusion of pelvic organs, which causes discomfort and function difficulty. The treatment for a pelvic floor prolapse is a sacrospinous ligament fixation procedure.
The procedure requires a disposable surgical device to apply specialized sutures to the ligaments deep within the pelvis, Nardos said. Surgeons can use the device to apply the sutures safely without having to visualize the ligaments inside the pelvis, which prevents any risks that might occur like bleeding.
The new device differs from the current tools available in the U.S. because it is made of metal instead of plastic, which can be easily reused when properly sanitized, according to Nardos. The device also uses regular sutures that are readily available in low- to middle-income countries, instead of specialized sutures.
Disposable medical devices make a lot of money for companies, but they increase health care costs and produce waste, Nardos added. Current devices are out of reach.
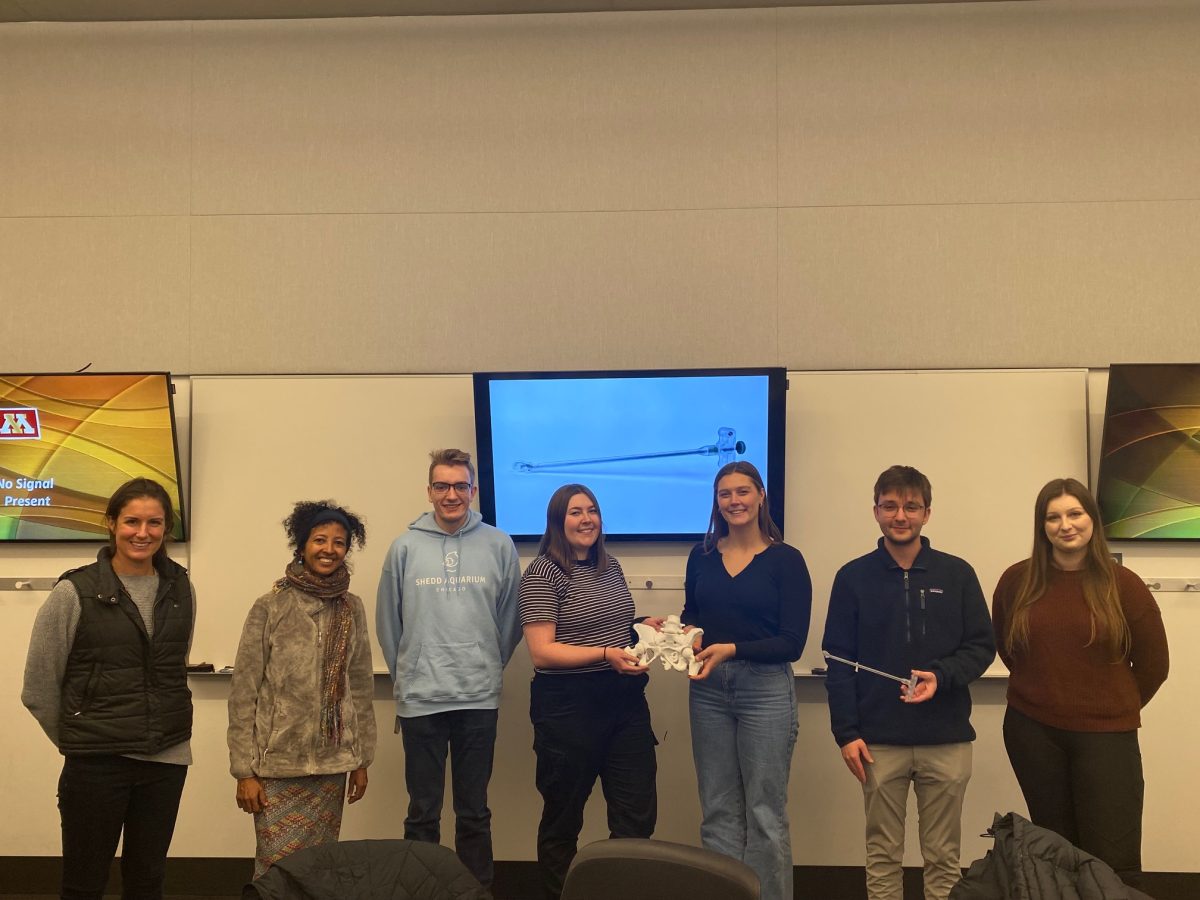
Nardos said she pitched the idea to the director of the Institute of Engineering and Medicine in 2021, who referred her to the new product and business development course. The idea was approved and Nardos was assigned six students and a faculty member to help develop the prototype.
Tinen Iles, an assistant professor in the Department of Surgery, learned about the project while teaching the new product and business development course and asked to be a part of the research.
Iles said she helped conduct voice-of-customer interviews, submit a patent, complete the final design and manage the six students involved in the project.
Voice-of-customer interviews are part of the design process, Iles said. Researchers interview potential customers about the product and use the feedback to make any necessary changes to the prototype.
For the pelvic floor tool, Iles said they interviewed five to six surgeons in Ethiopia. Iles and her team asked the surgeons questions about what they liked about the product, what they would want to change and if the device was easy to use.
“The students gave energy to the whole process by seeing their excitement for making a difference,” Iles said.
Josh Augustine, a business graduate who was in the new product and business development course, helped develop the business model.
When developing the business model, Augustine said they had to consider the humanitarian aspect of the product and how much fundraising is needed to get the product into physicians’ hands.
“I love this project because we are genuinely helping people and equipping physicians with this tool,” Augustine said.
Augustine said he stayed on after the course ended to help bring the product to market. He has acted as a liaison for undergraduate students in a senior engineering class, who refined the features of the prototype in the second year of its development. He was also the student representative for Nardos when she was applying for grants and attending events.
The tools currently being used in Africa to treat pelvic floor prolapse are hard to use and old, Augustine said.
“It’s arguably unethical. These people wouldn’t be getting this device without Nardos and the program,” Augustine said.
The device currently has a provisional patent, Nardos said. Within the next year, she said she hopes they will have finished the alpha prototype and begun cadaver testing.
“We are doing one step at a time,” Nardos said.











Jennifer Rupert
Apr 9, 2024 at 11:49 pm
Rahel continues to amaze and excel in service to others – proud to know you! – a former colleague