Researchers at the University of Minnesota College of Pharmacy partnered with the Minnesota Department of Health (MDH) to map out where pharmacies are across Minnesota.
The researchers mapped pharmacies, identified challenges communities face when they lose a pharmacy and informed people about the problem since 2020. As they continue their research, the group hopes to educate the public about pharmacy closures.
Lindsay Sorge, the senior strategic initiatives lead on the project and an assistant professor in the College of Pharmacy, said MDH and the Minnesota Board of Pharmacies compiled a list of pharmacies around the state to refer to and confirm they were open to ensure the map is accurate.
“We called pharmacies and said, ‘Are you still open? You’re not coming up on our pharmacy list,’ and sometimes found they moved across the street,” Sorge said.
Sorge said they also did this to confirm the pharmacies were brick-and-mortar stores open to the community and not mail-order pharmacies or pharmacies inside hospitals.
Moving forward, team members are working to find ways to share the map with others, Sorge said.
“It’s not just like detecting it and leaving it and walking away,” Sorge said. “It’s like understanding and then picking up on the advocacy piece.”
Sarah Westberg, associate dean of professional affairs and professor in the College of Pharmacy, said pharmacies tend to close for financial reasons. She said pharmacies do not get adequate reimbursement from insurance companies for medications and staffing.
“Many times, insurance companies and pharmacy benefit managers are reimbursing pharmacies at a rate that is less than it costs them to dispense the medication,” Westberg said.
Chrystian Pereira, an associate professor at the College of Pharmacy, said the low reimbursement rates make it difficult for pharmacies to stay in business.
Pereira said when mapping pharmacy gaps around the state, they needed to use different ways to measure gaps in rural versus urban areas.
“One of the things we did in our project was coming up with a definition to fit those different places,” Pereira said. “And then we didn’t measure the distance like if you put a ruler on a map from one place to another place, we measured your traveling distance. So how far would someone have to drive to get to a pharmacy and then we let that kind of distance create our definition.”
Traveling five miles in urban areas to get to a pharmacy is different from traveling five miles in a rural area because things are more spread out, Pereira said. It is more common to travel longer distances for day-to-day needs in rural areas.
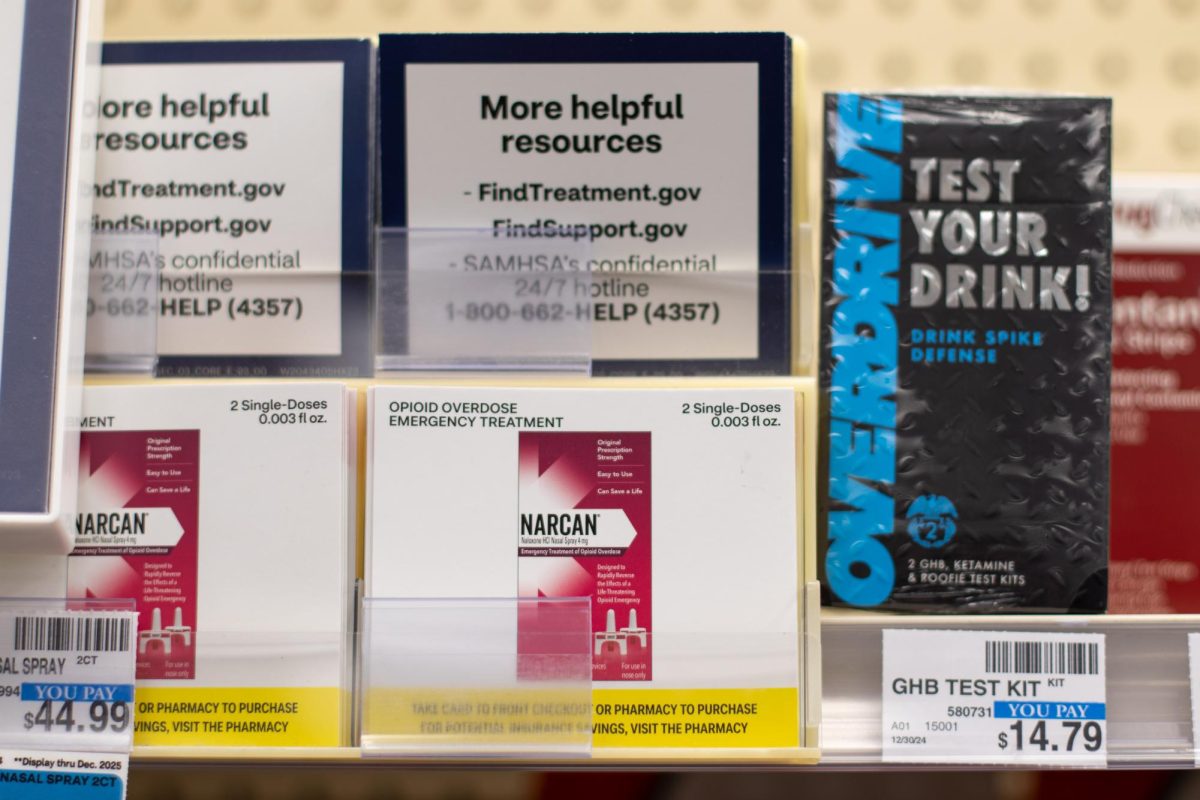
Westberg said pharmacies provide additional care like vaccinations and clinics outside of selling medications to help the community and to make a profit aside from selling prescriptions.
“A pharmacy is so much more than picking up a bottle of pills, they are the most accessible healthcare provider, usually on the entire healthcare team,” Westberg said. People go to pharmacies to ask questions about their situation to determine if they need to go to the emergency room or if they can treat themselves at home or to get feedback on what medications they need.”
Westberg said a large percentage of people go to pharmacies for vaccinations. When pharmacies close, people lose access to those additional services.
“You take that pharmacy out of there and deliver medication to the doorstep or in the mailbox of a patient, that doesn’t replace all those other services,” Westberg said.